Common Minerals: How do deficiencies and overdoses affect our health
Minerals play a vital role in overall health; If you consume too much or not enough, it can lead to serious health problems.
In 2025, Razzaque and S. Wimalawansa published a paper titled “Minerals and Human Health: From Deficiency to Toxicity (Minerals and Human Health: The “From Deficiency to Toxicity” review details the consequences of common mineral deficiencies and the risks of excessive intake, focusing on the large number of minerals calcium, magnesium and phosphorus because of their important physiological roles and associated metabolic pathways;
It also highlights the physiological functions of various trace minerals, including iron, zinc, selenium, iodine and copper, as well as some potential toxic effects in the body.
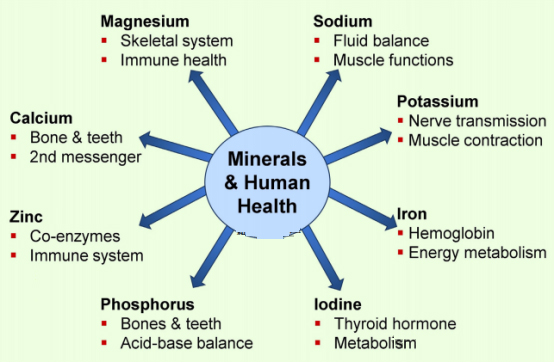
importance of minerals to human health
An adequate mineral balance is essential for maintaining normal health and preventing disease.
Minerals are essential for the maintenance of various physiological functions and can be divided into two broad categories:
(1) macroelements, mainly including calcium, phosphorus, magnesium, sodium and potassium;
(2) trace elements, such as iron, zinc, copper, iodine, selenium and manganese;
These minerals are essential for the growth and development of bones and teeth and for the physiological function of muscles and nerves.
Minerals help maintain fluid balance, regulate pH, and act as cofactors for many enzymes and coenzymes.
Specific mineral ions are involved in selective functions, from exerting antioxidant effects (selenium, zinc and copper) to producing hormones (iodine is used in thyroid hormones).
The consequences of deficiency and the toxicity of excess
Deficiencies in essential minerals can lead to serious health complications, including:
- Calcium deficiency → osteoporosis, fracture, muscle spasm, arrhythmia.
- Magnesium deficiency → Increased risk of muscle cramps, irregular heartbeat, osteoporosis, and metabolic disorders.
- Phosphorus deficiency → Weak bones, fatigue, muscle dysfunction, poor growth.
- Iron deficiency → anemia, cognitive impairment, immune dysfunction.
- Zinc deficiency → Delayed wound healing, impaired immune function, delayed growth.
- Iodine deficiency → goiter, hypothyroidism, gaseous cognitive impairment.
Conversely, excessive intake of these minerals can also be harmful, leading to the following conditions:
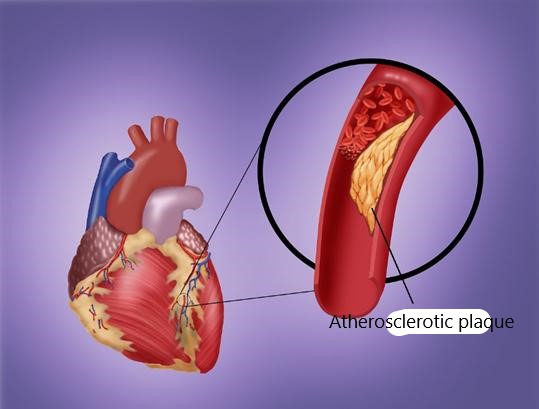
- Hypercalcemia → kidney stones, vascular calcification, arrhythmia.
- Hypermagnesia → hypotension, muscle paralysis, cardiac arrest.
- Phosphorus poisoning → Cardiovascular calcification, kidney damage, metabolic disorders.
- Iron overload → Organ damage, oxidative stress, increased risk of infection.
- Selenium poisoning → Hair loss, weak nails, nervous system damage.
Interaction of calcium, magnesium and phosphate
Calcium, magnesium, and phosphorus: These three minerals share an interconnected regulatory pathway, with parathyroid hormone (PTH), vitamin D, and fibroblast growth factor (FGF23) playing a key role in maintaining their balance.
Calcium and magnesium have an agonist-antagonist relationship in which an unbalanced Ca:Mg ratio (ideally 2:1) can lead to metabolic and cardiovascular disease.
Phosphate levels are tightly controlled to prevent excessive accumulation, which has been linked to kidney disease and cardiovascular problems.
Public health strategies for at-risk populations
Certain populations, such as pregnant women, the older people, vegetarians, and people with chronic diseases, are at higher risk of mineral deficiencies.
Public health initiatives should focus on diet education, food fortification and appropriate supplementation to prevent health complications.
Emphasis on diet-based solutions to combat mineral deficiencies, including:
- Increase consumption of nutrient-rich foods (e.g. dairy products, green leafy vegetables, nuts, seeds, seafood).
- Food fortification and biofortification (adding essential minerals to staple crops).
- Nutrition education and behavior change interventions.
- Supplemental programs, especially for high-risk groups.
Mineral level assessment in the body
Nutritional element analysis in functional medicine is an individual-centered health assessment method, the core of which is to reveal potential nutritional imbalances (such as deficiency, excess or metabolic abnormalities) by detecting and analyzing the nutritional status in the human body, so as to provide scientific basis for disease prevention, health optimization and chronic disease management.
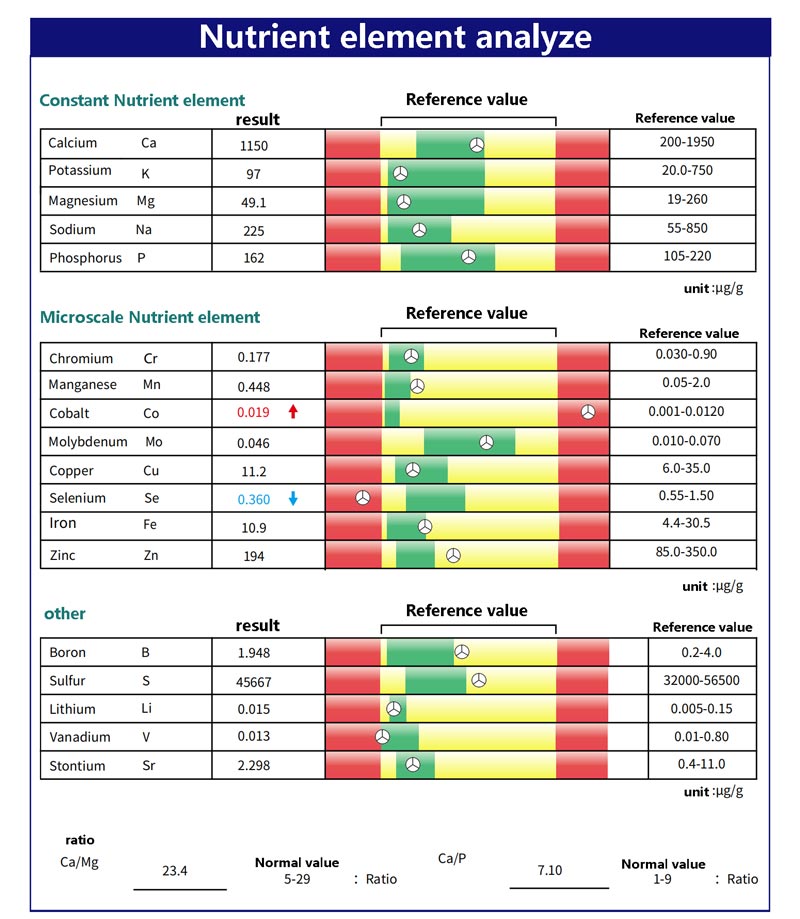
unscramble
Cobalt excess
1. Potential causes of excess cobalt
Exogenous exposure:
- Occupational exposure: Hard metal manufacturing (tungsten carbide cobalt alloy), ceramic/glass colorants.
- Medical sources: Some artificial joints (metal prostheses release cobalt ions from wear), vitamin B12 injections (rare).
- Diet or water contamination: crops grown in cobalt-rich soil or water sources in areas contaminated by industry.
Endogenous metabolic abnormalities:
Vitamin B12 metabolism disorders (e.g., methylmalonic aciduria).
Renal insufficiency leads to reduced excretion.
(2) Health risks of excessive cobalt
Thyroid toxicity: Inhibition of thyroid peroxidase activity, leading to hypothyroidism (TSH↑).
Heart damage: cardiomyopathy, arrhythmia (” cobalt heart disease “associated with metal prostheses).
Neurological symptoms: hearing loss, tremors, peripheral neuropathy.
Blood system: Polycythemia (rare).
(3) Coping strategies
Check the exposure source:
Occupational history assessment (exposure to hard metal dust).
Examine artificial joints or dental implants (MRI can detect metal ion release).
Test for cobalt in drinking water or diet (such as beer or foods from areas with high cobalt).
Medical intervention:
Removal of cobalt exposure sources (e.g. replacement of metal prostheses).
Chelation therapy (use of EDTA or DMPS in cases of severe intoxication, as directed by a physician).
Supportive measures:
Increase dietary fiber and antioxidants (such as vitamins C and E) to promote excretion.
Thyroid function (TSH, FT4), cardiac ultrasound and nerve conduction were monitored.
Selenium deficiency
(1) Common causes of selenium deficiency
Insufficient dietary intake:
Selenium content in crops is low in areas with low soil selenium (such as Keshan disease area in China and parts of Northern Europe).
Vegetarians or strictly limit animal foods (fish, viscera are high in selenium).
Malabsorption:
Inflammatory bowel disease (Crohn’s disease, celiac disease) or a history of gastric surgery.
Heavy metals such as mercury and lead competitively inhibit selenium absorption.
Increased demand:
Oxidative stress is increased in patients with chronic infections, autoimmune diseases (such as Hashimoto thyroiditis), and cancer.
(2) Health risks of selenium deficiency
Decreased immunity: susceptibility to infection and increased susceptibility to viruses (such as myocarditis caused by Coxsackie virus).
Thyroid dysfunction: Decreased GPx activity leads to accumulation of H2O2, which aggravates thyroid cell damage (especially Hashimoto thyroiditis).
Reproduction and development: male infertility (sperm motility ↓), fetal neurodevelopmental defects.
Cardiovascular risk: Keshan disease (cardiomyopathy), atherosclerosis (oxidized LDL↑).
(3) Coping strategies
Dietary Supplement:
Selenium-rich foods: Brazil nuts (1 serving 70-90 µg), tuna, oysters, eggs, sunflower seeds.
Fortified food: Selenium yeast tablets (dosage should be careful, the upper limit for adults is 400 µg per day).
Targeted supplement:
Concomitant thyroiditis: Selenomethionine (200 µg/ day) is suggested to reduce TPO antibodies.
When heavy metal load is high: selenium combined with chelating agents (such as selenium + glutathione mercury removal).
Monitoring and adjustment:
Regularly test whole blood selenium and GPx activity to avoid excess (symptoms of selenium poisoning: hair loss, brittle nails, garlic breath).
Combined detection of zinc and iodine levels (three synergistically affect thyroid function).
The co-existence of cobalt excess and selenium deficiency suggests priority screening for environmental or iatrogenic cobalt exposure and correction of selenium deficiency through diet and supplementation.
The synergistic toxicity of both may exacerbate oxidative stress and organ damage (especially in the thyroid and heart), requiring systematic intervention and long-term monitoring.
Sum up
M.Razzaque’s study highlights the importance of a balanced mineral intake to maintain health and prevent deficiencies and toxicities.
Although minerals are essential to human physiology, excessive supplementation can be harmful and dietary intake should be carefully managed.
Nutritional analysis in functional medicine not only fills the evaluation gap in the “disease-free” stage of traditional medicine, but also upgrades nutritional intervention from “insufficient supplement” to “optimization function” through the perspective of systems biology.
By accurately identifying the biochemical uniqueness of individuals, it can realize the transformation from symptom management to root cause repair, and ultimately promote the transformation of the medical model from disease treatment to health promotion.
reference
Mohammed S. Razzaque and Sunil J. Wimalawansa.Minerals and Human Health: From Deficiency to Toxicity.Nutrients 2025, 17(3), 454; https://doi.org/10.3390/nu17030454.