What is Coenzyme Q10?
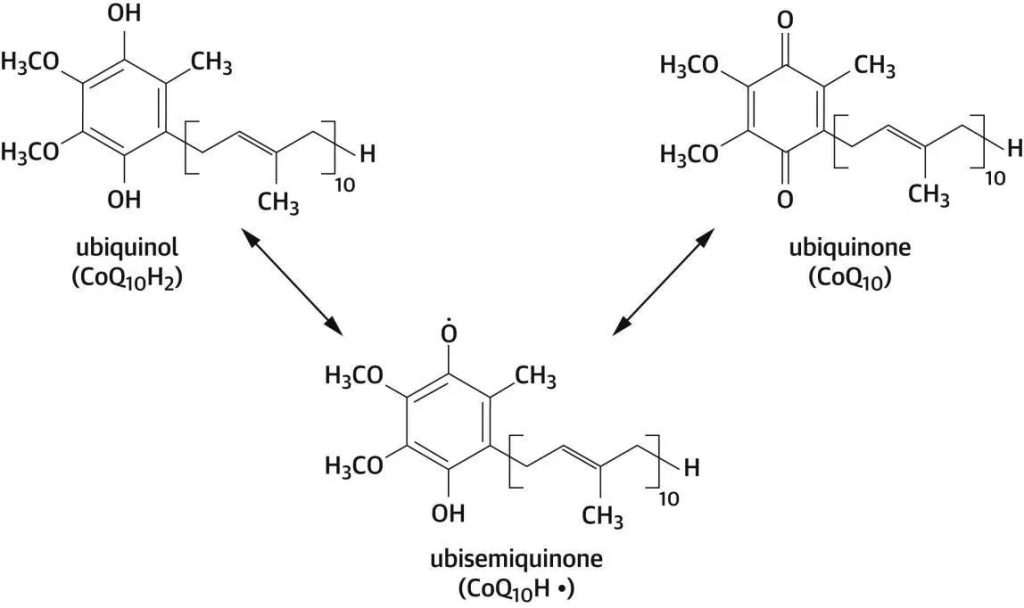
Coenzyme Q10 has three states: the fully oxidized ubiquinone form (Coenzyme Q10), the free radical semi-ketone intermediate (COQ10H), and the fully reduced ubiquinol form (COQ10H2), which can be converted into each other in the body.
A naturally occurring compound, widely distributed in animals and humans, first discovered in 1957 by Professor Frederick Crane and his colleagues in the United States, whose name derives from its chemical structure, with the benzoquinone ring as the main body and the side chain consisting of 10 isoprene units.
As one of the most commonly used nutritional supplements, Coenzyme Q10 is involved in the production of ATP, which plays an important role in bioenergy generation, and has been widely used in cardiovascular and reproductive fields.
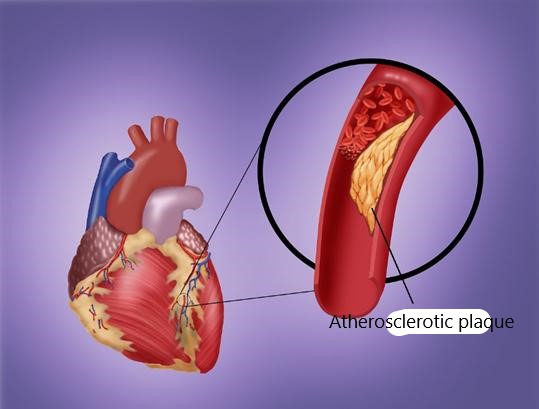
Heart Failure
Heart failure is a group of syndroes in which ventricular filling and ejection function are impaired due to various cardiac structural functional diseases, cardiac output can not meet the needs of body tissue metabolism, pulmonary circulation and systemic circulation congestion, and organ and tissue blood perfusion insufficiency are clinical manifestations.
1. Main symptom
These include difficulty breathing, limited physical activity and fluid retention.
When the disease worsens, symptoms such as lung congestion, shortness of breath, chest tightness, edema of both lower limbs, weakness and dizziness may appear
2. Clinical routine treatment
Symptomatic supportive treatment is performed with diuretics, angiotensin converting enzyme inhibitors, beta blockers and aldosterone receptor antagonists. On this basis, coenzyme Q10 and trimetazidine can be used as adjuvant therapy.
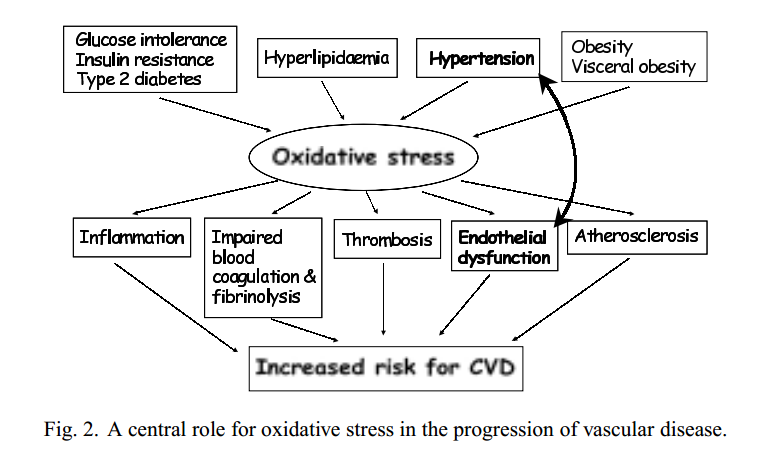
3. Pathophysiology – oxidative stress
Oxidative Stress (OS) plays a central role in the pathogenesis of cardiovascular diseases, including heart failure and hypertension.
Heart failure is often characterized by a loss of systolic function resulting from an energy-depleted mitochondrial state, which is associated with low levels of endogenous coenzyme Q10.
Coq10 deficiency has been demonstrated in endocardial biopsy samples from patients with cardiomyopathy, and the deficiency of coQ10 is associated with the severity of the disease, suggesting that coQ10 treatment can improve the quality of life of patients with heart disease by enhancing myocardial contractility.
Many studies have investigated the benefits of Coenzyme Q10 supplements to improve cardiovascular function by enhancing energy production, improving myocardial contractility, and its powerful antioxidant activity, particularly to prevent LDL oxidation.
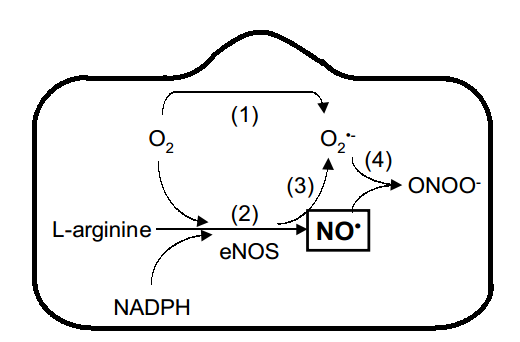
The mechanism of coenzyme Q10 in vascular oxidative stress
- (1) Inhibition of mitochondrial production of superoxide (O2-)
- (2) Recoupling eNOS activity by maintaining cellular NADPH concentration
- (3) Further reduce the production of O2-
- (4) Reduce the oxidative catabolism of NO• peroxynitrite (ONOO−)
The end result will be to maintain endothelial cell NO• production, dilate blood vessels, and enhance biological activity, thereby improving endothelial dysfunction and blood pressure.
meta-study
1. meta-analysis
All the included literatures included 13 Chinese literatures and 14 English literatures. A total of 27 randomized controlled trials (RCTs) were included, including 3222 patients, including 1625 patients in the experimental group and 1597 patients in the control group. The maximum sample size was 641 cases and the minimum was 12 cases.
The included patients ranged in age from 24 to 101 years old. The control group received conventional Western medicine treatment, and the experimental group received oral coenzyme Q10 therapy on the basis of the control group for 1 to 24 months. The related indexes of heart failure were analyzed.
2. Research result
(1) Case fatality rate: A total of 11 studies were included, including 2083 patients, among which 1042 patients in the experimental group and 1041 patients in the control group.
The results showed that the case fatality rate of Coenzyme Q10 group was better than that of the control group, and the difference was statistically significant (P = 0.0006).
(2) Ejection fraction: Twenty studies included, including 2041 patients, including 1023 patients in the experimental group and 1018 patients in the control group.
The results showed that the ejection fraction of Coenzyme Q10 group was better than that of the control group, with statistical significance (P < 0.00001).

Further subgroup analysis by race showed that:
The ejection fraction of coenzyme Q10 group in Chinese population was better than that in control group, the difference was statistically significant (P < 0.00001).
There was no significant difference between the two groups in non-Chinese population (P = 0.36).
(3) NYHA grading: A total of 4 studies included, including 218 patients, among which 111 patients in the test group and 107 patients in the control group.
The results showed that the cardiac function grading in the Coenzyme Q10 group was lower than that in the control group, with statistical significance (P < 0.00001).
(4) 6-minute walking distance (6MWT) : 10 studies included, including 1077 patients, including 547 patients in the experimental group and 530 patients in the control group.
The results showed that 6MWT in coenzyme Q10 group was better than that in control group, and the difference was statistically significant (P < 0.00001).
(5) Adverse reactions: Six studies reported adverse reactions.
The main manifestations of adverse reactions were peripheral arterial vascular events, deep vein thrombosis, stroke,
possible or eventual myocardial infarction, coronary artery bypass grafting, percutaneous coronary intervention, arrhythmia, chest pain, gastrointestinal dysfunction, etc.
The results showed that the adverse reactions of coenzyme Q10 group were lower than those of control group.
3. Research conclusion
The application of Coenzyme Q10 in patients with heart failure can reduce mortality,
improve NYHA cardiac function grade, increase ejection fraction, improve 6MWT, and has a good safety.
Coenzyme Q10 recommended as an adjunct therapy, which can improve myocardial energy metabolism in patients, thereby improving heart function.

Expert consensus on the application of Coenzyme Q10 in patients with cardiovascular diseases
In 2021, the Journal of the American College of Cardiology (JACC) published an expert consensus on the Use of Coenzyme Q10 in Patients with cardiovascular disease.
In vivo, Coenzyme Q10 synthesized via the mevalonate pathway, an essential metabolic pathway whose byproducts include cholesterol and other isoprene.
It is precisely because the mevalonate pathway determines the synthesis of a variety of metabolites in the body that coQ10 plays an important role in cardiovascular disease.
To date, no consensus has established on the minimum or maximum effective dose of coQ10.
In heart-related trials, doses of 100 to 400 mg per day typically used, while in neurodegenerative diseases such as Huntington’s disease,
Parkinson’s disease, and amyotrophic lateral sclerosis, studies use doses ranging from 600 to 3,000 mg.
Sum up
Coenzyme Q10 mainly exists in the mitochondria of animals and humans.
As one of the most commonly used nutritional supplements, it participates in the production of ATP,
provides energy for the body, and plays an important role in the generation of biological energy.
At present, it has widely used in cardiovascular and reproductive fields.
Since the discovery of coenzyme Q10, its application in cardiovascular medicine has been in full flow, and the heat has been rising.
A domestic meta-analysis showed that coenzyme Q10 can reduce the mortality of patients with heart failure,
improve NYHA cardiac function classification, increase ejection fraction, improve 6MWT, and has a good safety.
Studies have also shown that oxidized CoQ10 replaces reduced CoQ10 to treat and prevent cardiovascular disease in patients with heart failure.
Relevant guidelines at home and abroad also clearly point out that coenzyme Q10 can improve patients’ myocardial energy metabolism,
thereby improving heart function, and the recommended dose for heart disease is 100 to 400 mg per day.
References:
- [1] Tan Yunze, Fan Zongjing, Cui Jie, et al. Efficacy and safety of Coenzyme Q10 in the treatment of heart failure [J]. Research on Drug Evaluation, 2019,46(11):2432-2443. (in Chinese) DOI:10.7501/j.issn.1674-6376.2023.11.021.
- [2].Hodgson, Jonathan M, and Gerald F Watts. “Can coenzyme Q10 improve vascular function and blood pressure? Potential for effective therapeutic reduction in vascular oxidative stress.” BioFactors (Oxford, England) vol. 18,1-4 (2003): 129-36. doi:10.1002/biof.5520180215.
- [3].Hodgson, Jonathan M, and Gerald F Watts. “Can coenzyme Q10 improve vascular function and blood pressure? Potential for effective therapeutic reduction in vascular oxidative stress.” BioFactors (Oxford, England) vol. 18,1-4 (2003): 129-36. doi:10.1002/biof.5520180215.
- [4]. Chinese expert consensus on diagnosis and treatment of fulminant myocarditis in adults [J]. Clinical Medicine Research and Practice,2018,2(32): Feng 3.
- [5]. Chinese Medical Association Branch of Cardiology, Chinese Medical Doctor Association Branch of Cardiovascular Physicians, Chinese Medical Doctor Association Heart Failure Professional Committee, et al. China heart failure diagnosis and treatment guidelines 2024 [J]. Chinese journal of cardiovascular disease, 2024,52 (3) : 235-275. The DOI: 10.3760 / cma. J.c. n112148-20231101-00405.
- [6].Raizner, Albert E, and Miguel A Quiñones. “Coenzyme Q10 for Patients With Cardiovascular Disease: JACC Focus Seminar.” Journal of the American College of Cardiology vol. 77,5 (2021): 609-619. doi:10.1016/j.jacc.2020.12.009
- [7].Judy, William V. “The Instability of the Lipid-Soluble Antioxidant Ubiquinol: Part 2-Dog Studies.” Integrative medicine (Encinitas, Calif.) vol. 20,5 (2021): 26-30.